
The most common degenerative-dystrophic disease of the spine is osteochondrosis. Its peculiarity is that it does not manifest itself in any way in the initial stages, so many patients turn to the doctor when the processes of tissue destruction have already gone too far. But even in this case, the diagnosis is not made immediately, but after a series of laboratory and instrumental examinations. It is very important to correctly diagnose osteochondrosis, because the earlier treatment is started, the greater the possibility of preventing complications. For this reason, you must recognize the symptoms of osteochondrosis in time and consult a doctor.
Causes and mechanism of development
Osteochondrosis begins with destructive processes in the intervertebral discs. They gradually dry and reduce in volume. This leads to the fact that the disks can no longer perform their functions properly. They can collapse and then develop a hernia. But most often this condition leads to the development of osteochondrosis.
After all, the intervertebral disc protects the vertebrae from destruction, serves as a shock absorber during various movements and keeps the vertebrae in the correct position. As its volume decreases, the vertebrae move. The instability of one segment of the spine leads to the formation of osteophytes - bone growths that keep the vertebrae apart. Otherwise, pinching of nerve roots and compression of blood vessels can occur. All these processes cause the presence of many different signs of osteochondrosis, which is why it is so difficult to diagnose it in time. But if you know why this pathology develops, people at risk can be more careful.
Osteochondrosis is usually caused by the following reasons:
- congenital disorders in the development of the spine or connective tissue defects;
- injuries or constant overload, heavy physical work;
- bad posture, flat feet, wearing uncomfortable shoes;
- prolonged stay in an uncomfortable position, sedentary lifestyle;
- obesity, poor nutrition, excess weight;
- exposure to chemicals, for example, bad habits, taking certain medications;
- frequent stresses;
- natural processes that occur during the aging of the organism;
- constant vibration effect on the spine.
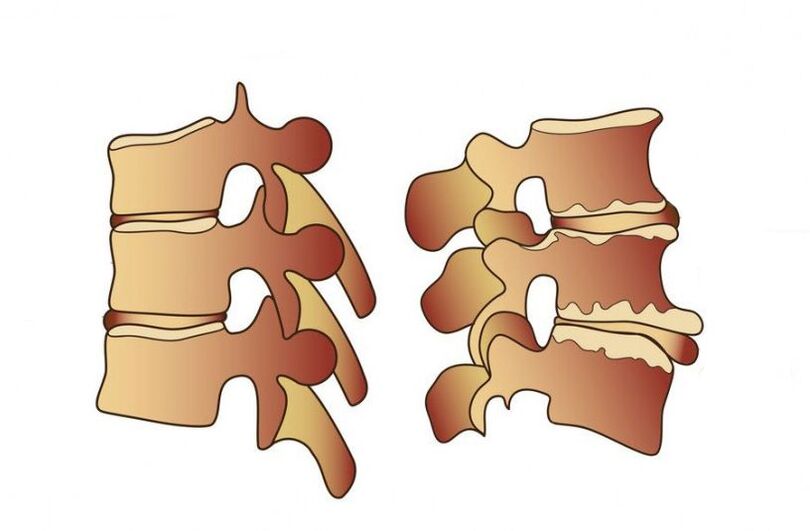
Osteochondrosis develops after a decrease in the height of the intervertebral disc, after which the vertebrae themselves begin to collapse
Therefore, it is necessary to carefully monitor your health in order to consult a doctor at the first symptoms. This is especially important for athletes, loaders, drivers, gymnasts, women, who often worry about their loved ones and therefore experience stress.
Symptoms
Signs of osteochondrosis depend on the stage of the disease, as well as on which part of the spine is affected by degenerative processes. Very often at first the patient does not even feel back pain, only a slight stiffness in the morning. In the process of destruction of the intervertebral disc due to displacement of the vertebrae, nerve roots are compressed and pain occurs. Depending on the location of the disease, they can appear not only in the back area. Often the pain radiates to the shoulder blade, chest, arm or leg, and it can also be a headache.
A characteristic of osteochondrosis in the initial stages is that the pain increases with physical activity and subsides after rest. Even after taking a comfortable body position, the patient feels better. Painful sensations worsen after hypothermia, stress, prolonged stay in a static position, for example, when working at the computer or while sleeping on an uncomfortable bed. Very often, stiffness of movements, muscle weakness and constant fatigue are observed in osteochondrosis. The patient tries to take a comfortable position in which he feels less pain.

The main sign of lumbar osteochondrosis is pain and stiffness in movement.
Symptoms of lumbar osteochondrosis
The most common location of degenerative-dystrophic processes is the lumbar spine. It can withstand the greatest loads not only when moving, but also when a person sits in one position for a long time. Due to the sedentary lifestyle of modern people, the muscle corset here is weak, so any overload can lead to the destruction of the discs or displacement of the vertebrae.
In addition to pain and general stiffness, there are special symptoms of osteochondrosis of the spine in the lumbar region. If the following signs appear from time to time, it is necessary to make an appointment with a neurologist:
- lower limbs go numb;
- skin sensitivity is impaired, paresis may develop;
- pain is felt in the pelvic organs, their functioning is disturbed;
- the patient cannot turn or bend, the pain is felt even when sitting.
Symptoms of cervical osteochondrosis
It is especially important to know what symptoms the patient experiences with cervical osteochondrosis. After all, sometimes the pain in the neck is not even felt, and the other symptoms are similar to vascular disorders that a person tries to treat with drugs. If the destructive processes in the cervical spine are not stopped, it can lead to disruption of the blood supply to the brain and even complete paralysis of the body.
Therefore, it is very important to pay attention to the following signs in time:
- headaches that cannot be relieved by conventional analgesics;
- dizziness occurs when turning the head;
- pain can be felt in the shoulders, back of the head, hands;
- vision deteriorates, spots or colored spots are visible in front of the eyes;
- there is hearing loss, tinnitus;
- tongue and fingers numb;
- movement coordination is disturbed.

Headache and tinnitus often occur with cervical osteochondrosis
Symptoms of thoracic osteochondrosis
Signs of osteochondrosis in the thoracic region are easily confused with diseases of internal organs. And although the main symptom is back pain, it has its own characteristics. Patients describe this feeling as if the chest is being squeezed by a hoop. The pain intensifies when inhaling and exhaling, so many attribute these feelings to heart pathologies.
With thoracic osteochondrosis, the pain will increase with hypothermia, raising the arms up, and also at night. You may feel numbness of the skin, goosebumps and coldness of the extremities. Disturbances in the work of the digestive system often occur.
Diagnostics
To prevent complications of osteochondrosis, it is very important to consult a doctor as soon as its first signs appear. It is stiffness in movement and back pain after exercise. This pathology is treated by a vertebrologist or a neurologist. An experienced doctor can make a preliminary diagnosis during the examination and conversation with the patient.
But some symptoms of the disease are very non-specific and resemble the manifestations of many other pathologies. Therefore, differential diagnosis is very important, which will help to rule out diseases in which both vascular and neurological symptoms develop. It can be angina pectoris, hypertension, peptic ulcer, pyelonephritis. The main difference between osteochondrosis and them is that it has a chronic course and develops slowly, with periodic exacerbations, and the pain usually disappears at rest.
But without special diagnostics it is still difficult to make a correct diagnosis. Instrumental examination methods are most often used for this: radiography, CT, MRI, ultrasound, myelography and others. Sometimes laboratory tests may also be necessary. They will help identify the presence of an inflammatory process and an increase in the concentration of calcium in the blood.

The most common diagnostic method in the initial stage of the disease is radiography.
Radiography
In the initial stage, X-ray diagnostics are needed to confirm the diagnosis. This is the main method of examination for osteochondrosis. It is the simplest and most affordable and has the fewest side effects. After determining the location of the pain, photographs are taken of this area of the spine. They are usually performed in two projections: direct and lateral.
If the diagnosis is correctly established, the following radiological signs will indicate it: the distance between the vertebrae is reduced, atrophy of the intervertebral discs is observed, osteophytes are visible, destruction of the vertebrae or a change in shape may occur. spinal column.
myelography
This is a more complex method, can have side effects and is not suitable for everyone. After all, myelography is based on injecting a special contrast liquid into the spinal canal. This can cause an allergic reaction or even damage to the spinal cord. After that, an X-ray of the spine is taken.
This method allows you to examine the spinal canal and determine where it is damaged by degenerative processes. In addition, myelography can determine the presence of intervertebral hernias in the initial stage.

MRI is a more informative examination method, so it is used when a differential diagnosis is necessary.
Tomography
Diagnosis of osteochondrosis using CT or MRI is performed less often, because these methods are not yet available everywhere. Therefore, they are used in severe cases, as well as if it is necessary to distinguish osteochondrosis from other diseases. But with an MRI or CT scan, you can examine the spine and surrounding tissues in detail.
These diagnostic methods allow you to see the condition of blood vessels, the presence of hernias, compression of nerve roots and the shape of intervertebral discs. They are necessary for the differential diagnosis of osteochondrosis from osteomyelitis, spinal cord tumor, spondylitis, ankylosing spondylitis and syringomyelia.
Timely recognition of the symptoms of osteochondrosis and its correct diagnosis will help to start treatment on time. This will prevent the development of complications, alleviate the patient's condition and reduce the number of exacerbations.

















































